Hip Fracture In Old Age
Why do elderly people have hip fractures?
The reason why elderly people are more prone to hip fractures includes the occurrence of contributing factors that include a decline in bone density, loss of muscle strength, and imbalance; this contributes to an increased tendency to fall. Other age-related factors include poor eyesight or medications leading to dizziness, which can make them more likely to fall and hence fracture some bones.
What are the symptoms of hip fracture among the elderly?
Symptoms often include severe pain in the hip or groin, inability to stand on the involved leg, and unable to stand or walk. Some individuals also show bruising, swelling, and outward turning of the affected leg. If the fracture is not that serious, the pain may not be that great, but hip pain after a fall should receive medical attention.
What are the choices concerning hip fracture treatment in elderly patients?
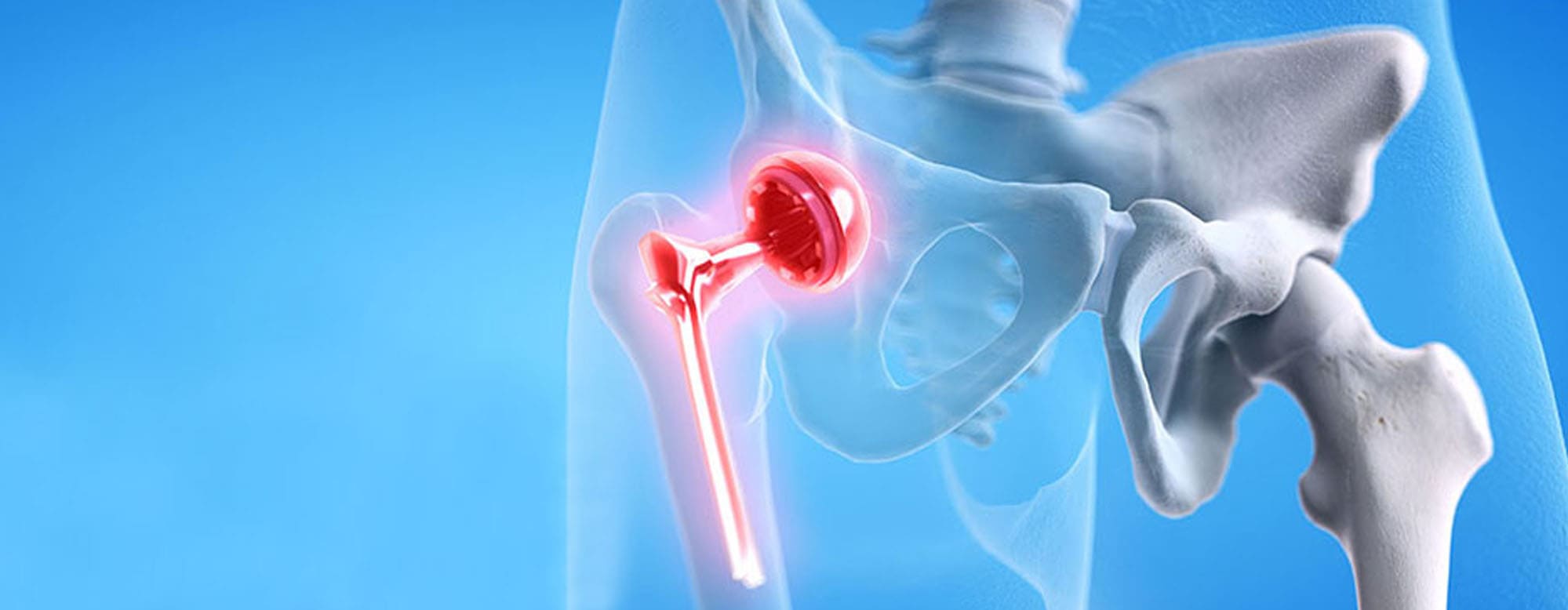
Treatment usually involves surgery to repair or replace the fractured hip. Options include internal fixation, where metal screws or plates are used; partial hip replacement; or total hip replacement, depending on the type of fracture and overall health of the patient. Often, surgery is followed by physical therapy and rehabilitation for assistance in recovery and mobility.
What does the road to recovery look like following a hip fracture for older adults?
Recovery depends on the patient’s age, health condition, and type of fracture. Treatment is generally based on physical therapy to regain muscle strength, balance, and mobility. Some patients may require temporary or long-term aid in walking or daily activities. Recovery can take several months, and many people will experience lingering effects such as reduced mobility or increased risk of future fractures.
How do you prevent hip fractures among older adults?
Prevention of hip fracture involves the reduction of risk factors for falls and the improvement of bone health through exercises to maintain strength and balance, a diet containing calcium and vitamin D, medication to enhance bone density where this may be necessary, and modifications around the home to make it safer. Regular checks on vision and reviews of medications can also minimize risks of falls.